Released 6 November 2023
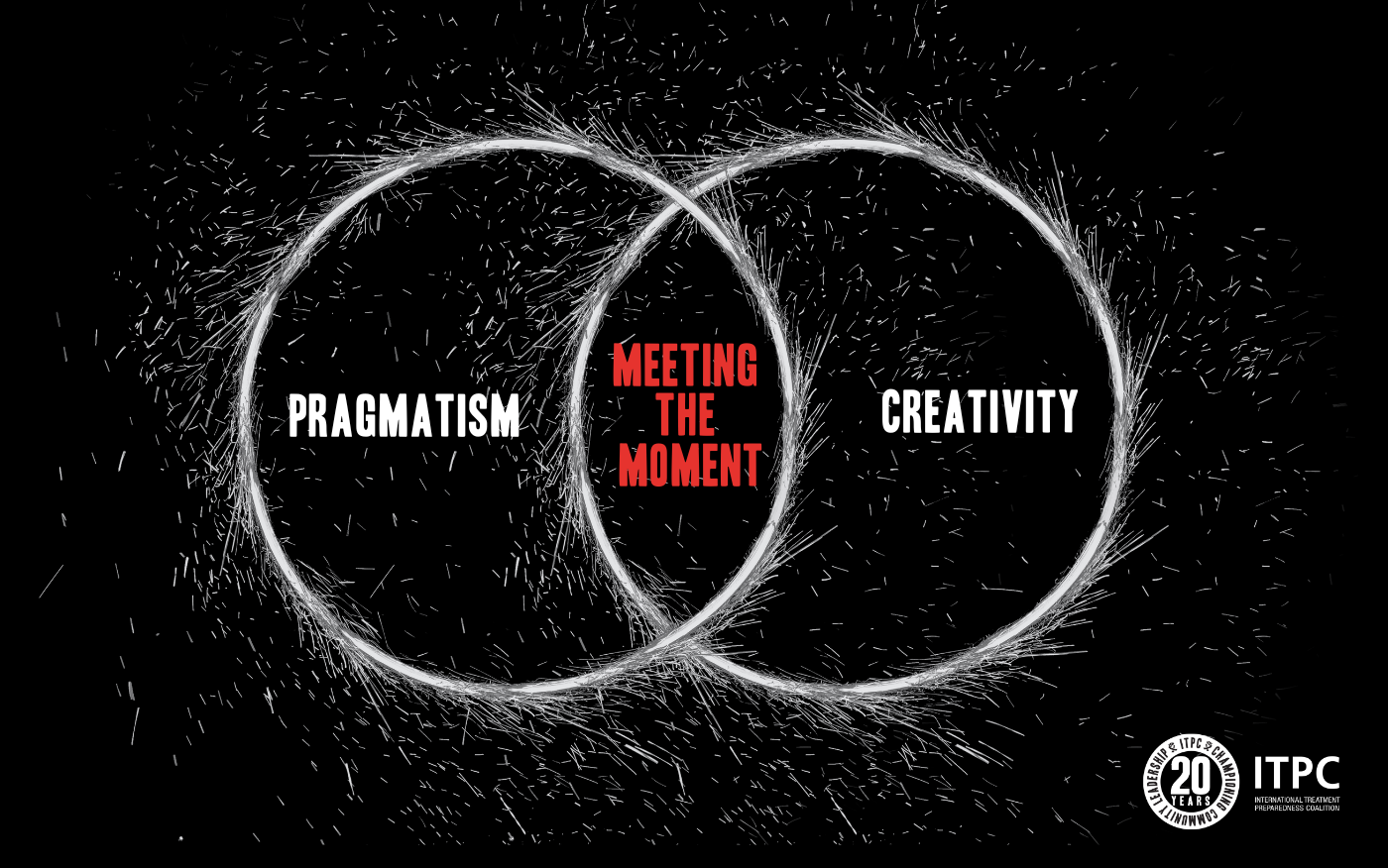
With new pandemics looming due to climate change and dwindling health budgets, the fight against AIDS is at a critical juncture. To preserve the gains made over four decades, we must be both creative and pragmatic. What trade-offs are we willing to make in a world with rising challenges and limited resources? How can we transition from an emergency AIDS response to a sustained one, globally?
The brief outlines five essential interventions to end AIDS as a public threat: 1) increase and sustain community data generation efforts, 2) address the critical healthcare worker shortage, 3) incorporate human rights into planning models, 4) tackle the rising cost of health products head-on and 5) overhaul the outdated global public health financing model.
Data
With the expected decline in global HIV prevalence, traditional population-based surveys will likely become less cost effective and not fit to provide the granular data necessary to guide the future HIV response. It is critical therefore, that we increase and sustain community data generation efforts to address the need for timely, nuanced data for decision-making. We can achieve that by investing in community systems that enable robust community-led interventions such as community-led monitoring (CLM). Effective CLM offers community-relevant data, identifies specific issues swiftly, generates data to back the required changes, and ultimately works with all stakeholders to co-create solutions.
Human Resources
The public health workforce crisis is more than just a staffing issue; it is deeply connected to the quality of services as experienced by recipients of care. While significant resourcing and attention are rightly placed on biomedical solutions, the crucial importance of effective management to address quality of service issues—rooted in sound operational and human resources practices—is under-explored. With tightening health budgets, specialized clinics that cater solely to specific groups (like sex workers or youth) may become less viable. Shouldn’t we strive for universally welcoming, high quality health services? Good service is friendly to all! Quality of service plays a pivotal role in patient retention and health-seeking behavior. Research shows that patients were willing to wait 19 hours more or travel 45 km farther to see nice rather than rude providers. Prioritizing better staff management and accountability is a critical yet overlooked strategy to address the dual challenges of human resources for health and service quality. Let’s remember that good management saves lives!
Human Rights
Bad laws kill. Discriminatory laws limit access to life-saving interventions like PrEP (pre-exposure prophylaxis), PEP (post-exposure prophylaxis) and vital services like harm reduction. While epidemiological and investment models must recognize these structural barriers, merely acknowledging them isn’t enough. Real change is contingent upon sustained advocacy for law and policy reform. It requires funding and targeted action at local and national levels to ensure that the voice of impacted communities influences the policies that affect their literal lives.
Affordability
Escalating costs of commodities and therapeutics, fueled by a global recession, rising inflation and excessive pricing by manufacturers, are pushing health budgets to the brink. Inequities are stark; some countries face much higher prices for the same products or lack access due to market manipulation. In an environment where every dollar counts and needs are ever-increasing, a strategic overhaul is crucial. The answer lies in intellectual property law reforms and incentivizing local manufacturing to reduce the reliance on monopolies. We must advocate for a people-first ecosystem that prioritizes health over profit and encourages local production, especially in the continent of Africa.
Health Financing
Funding challenges for HIV can’t be separated from the broader health financing crisis. They are inextricably linked to the wider common goods problem that manifests in a persistent $4.2 trillion funding gap per year for our Sustainable Development Goals. As many affluent countries lean to nationalism, traditional donor funds are diminishing or are at best, under threat. This dynamic puts a significant strain on lower-income country budgets, risking a reversal of progress achieved by initiatives like PEPFAR and the Global Fund. The sustainable path forward lies in Global Public Investment (GPI). By adopting an “all contribute, all benefit, all decide” approach, we not only sustain health financing but also democratize its implementation and structures.