In June, PLHIV (People Living with HIV) networks across the country started witnessing an acute shortage of certain Antiretroviral (ARV) drugs in Anti-Retroviral Therapy (ART) centres. Among them were pediatric formulations and dolutegravir, the backbone of HIV treatment.
READ MORE: We are suffering. Someone is not doing their job.
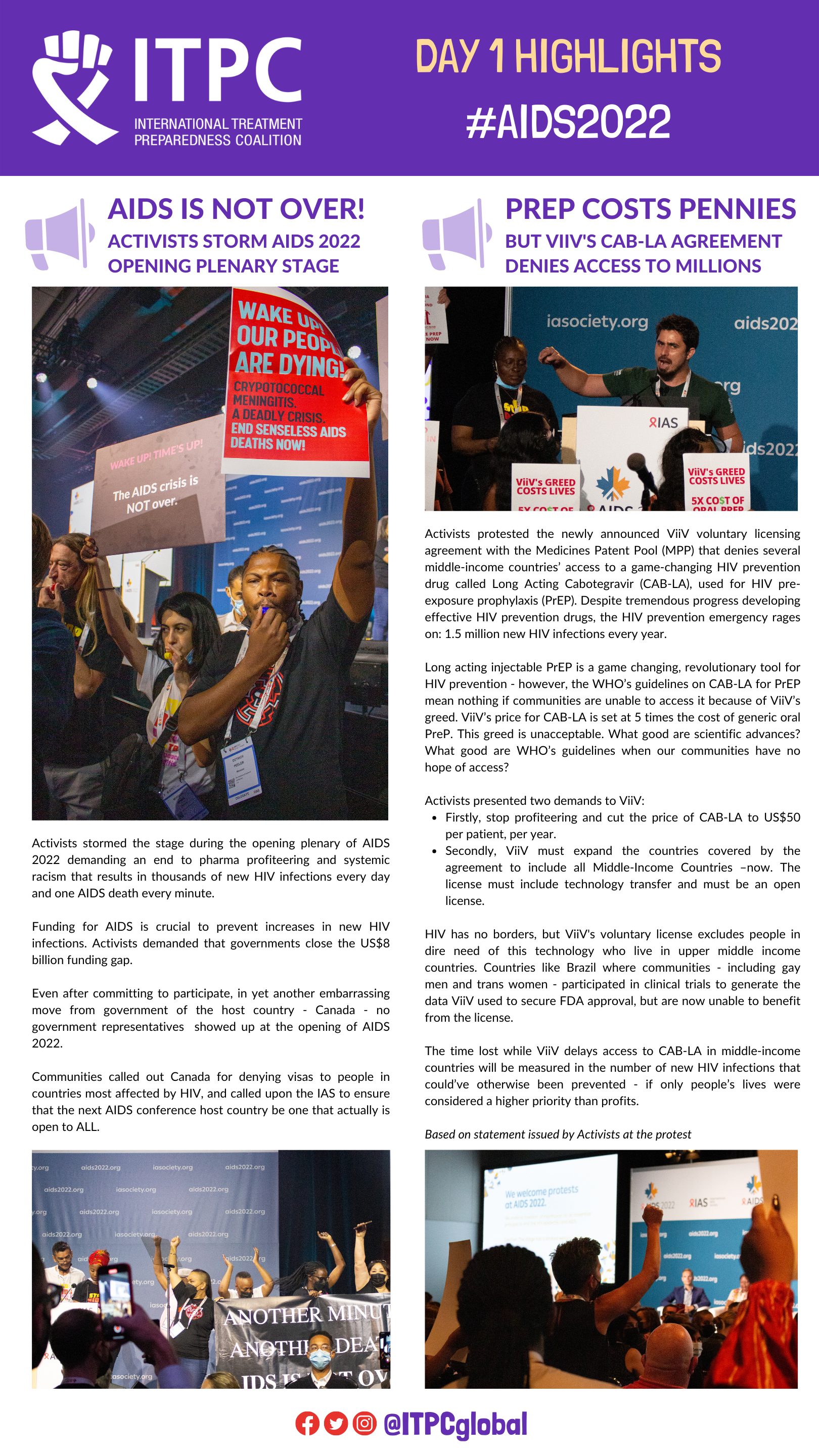
In the summer heat, PLHIV have been protesting peacefully for the past 23 days continuously on the premises of the National AIDS Control Organisation (NACO). The dharna (peaceful protest) is calling attention to the need for emergency procurement of ARVs and the unintended consequences of a weak and ineffective supply chain.
Suppressing virus
People living with HIV need access to treatment with a combination of drugs known as antiretroviral therapy to suppress the virus, preserve their health, and prevent transmission of the virus to an HIV-negative partner.
Staying on anti-retroviral therapy continuously is crucial to keep the virus suppressed. But the virus can mutate into a resistant form if treatment delivery is poor or patchy. As treatment activists, we have seen firsthand when antiretroviral therapy treatment is interrupted, people living with HIV develop resistance to their regimen and become vulnerable to life-threatening bacterial and fungal infections—the primary causes of hospitalisation and AIDS-related deaths in the community.
Governments such as the Indian government have made considerable advances in providing access to testing and antiretroviral therapy (ART) for people living with HIV. While there has been a reduction in AIDS-related deaths since 2004, progress has stalled in recent years, highlighting the need to ad-dress health system challenges such as disruptions in the medicine supply chain to end AIDS.
The disruptions in the lifesaving HIV medicine supply chain are not new. What drives these widespread re-occurring shortages in the last decade affecting many States is the failure of the pooled procurement mechanism. The National AIDS Control Organisation(NACO) under the Ministry of Health and Family Welfare is the nodal agency responsible for overlooking and coordinating activities of the National AIDS Control Programme (NACP) along with the Central Medical Services Society, which is responsible for centralised tendering and pooled procurement of different HIV products, including antiretroviral drugs.
The tender for pooled procurement of life-saving anti-retroviral medicines has faced bureaucratic delays in 2014, 2017, and now again in 2022.
Lack of treatment
A few days ago, NACO, in its public communication, claimed that 95% of PLHIVs have not faced any shortages. But by its own admission, the current shortages affect 5% of 14.5 lakh (1,450,000) people. People living with HIV report that ART centres are struggling to keep them on treatment.PLHIVs receive a minimum “one month’s dose” from ART centres.
Recently, they have had to make many trips in a month to get their pills, creating a chilling effect on adherence as poorer patients do not have the re-sources to travel frequently. Some have had their regimen changed due to the unavailability of certain ARVs and are worried if these changes are based on the World Health Organization’s guidelines and compromise their future treatment options.
Some PLHIVs have been asked to take multiple doses of pediatric formulations instead of adult formulations. As a result, the pill burden increases, and they worry that they may deprive a child living with HIV of their doses in the near future.
And when pediatric doses are not available, adult pills are broken or crushed, resulting in uneven dosing and an unpleasant taste that children do not like to take, making adherence challenging for caregivers.
The peaceful dharna in the NACO office seeks to get government attention on the timely tendering and procurement of HIV medicines and to hold accountable the health ministry’s procurement agency, the Central Medical Services Society, responsible for ARVs tenders to ensure an uninterrupted supply of life-saving treatment.
Shortages of health products in the supply chain of health programmes are not India’s problem alone and are commonly experienced in low-and middle-income settings. However, India has IT-enabled and community monitoring tools at its disposal.
Necessary actions
What is urgently needed is the political will from the Ministry of Health to take necessary measures to ensure that drug shortages, as happened over the last decade, are not experienced by its programmes, such as HIV and TB, in the future.
If ignored, the consequences impact the right to health and drive drug resistance, a significant public health challenge for the country.
(Leena Menghaney is a lawyer who works on medicines, law and policy.)

















 ITPC Life Maps assignments created spaces for me to reflect and process what was happening. I was able to help amplify the voice of ordinary people on what healthcare should look like; amplify solutions that come from real people inside communities the system is meant to serve.
ITPC Life Maps assignments created spaces for me to reflect and process what was happening. I was able to help amplify the voice of ordinary people on what healthcare should look like; amplify solutions that come from real people inside communities the system is meant to serve.
